Thromboangitis obliterans is a chronic disease seen predominantly in young male patients who smoke; it involves an inflammatory reaction of the arteries to nicotine. Initially, it becomes evident in the small arteries of the feet and hands and progresses proximally.
It results in vasoconstriction, decreased arterial circulation to the extremities, ischemia, and eventual ulceration and necrosis of soft tissues. The inflammatory reaction and resulting signs and symptoms can be controlled if the patient stops smoking.
PT(Physiotherapy) Management of Chronic Arterial Insufficiency
Plan of Care maybe include,
- To teach the patient how to minimize or prevent potential impairments and correct functional impairments or limitations which currently affect functional capabilities.
- Communicate with health professionals from other disciplines which are suitable for patient consultation.
- Improve exercise tolerance for ADL, and reduce intermittent claudication incidence.
- Relieve pain in repose.
- Prevents ulcerations in the skin.
- Enhance vasodilatation in arteries affected.
- Prevent or minimize joint contractures and muscle atrophy, especially when the patient is restrained to bed.
- Foster healing of any developing skin ulcerations.
A graded exercise program should be initiated for patients with mild to moderate arterial disease to improve exercise tolerance and functional capacity in day-to-day life activities. A regular program of aerobic exercise at a mild to moderate levels, such as walking or cycling, is known to have benefits for patients with chronic arterial insufficiency.
The demonstrated benefits include an increase in the time before the onset of exercise pain while walking, an improvement in the efficiency of oxygen use in muscle exercise (enabling patients to tolerate exercise over longer periods of time), and quantitative improvement in the quality of life. However, it is less clear whether the features of an optimal exercise program, or whether exercise programs improve collateral circulation in the extremities.
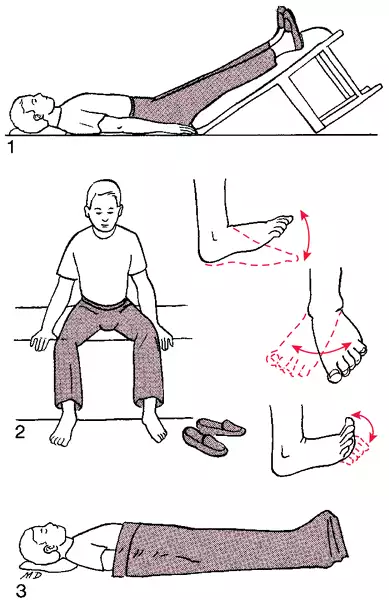
Another exercise approach developed several decades ago, Buerger or Buerger-Allen exercises were designed to promote collateral circulation through a series of positional changes of the affected limb (from elevated to dependent position) combined with active ankle pumping exercises.
Although frequently used in the past and occasionally today, there is little or no evidence to support the effectiveness of these exercises to improve the flow of blood to an extremity. There is little reason, therefore, to include them in an exercise program for a patient.
Special Considerations for Chronic Arterial Insufficiency Patients in a Graded Exercise Program
The rationale for graded exercise The following factors relating to the normal response of the body to exercise are the basis for using a graded exercise program to improve the functional status of chronic arterial insufficiency patients
1. Blood flow decreases temporarily during active muscle contraction but the blood flow increases rapidly immediately after the contraction.
2. After exercise cessation, the blood flow during the first 3 to 4 minutes is rapidly decreasing. This is followed by a slow decline within 15 minutes to the resting levels.
3. Blood flow in muscles can be increased with repeated moderate-level exercise beyond the resting blood flow values.
Exercise guidelines
- Patients should be encouraged to walk or cycle to a predetermined maximum target heart rate, but without causing intermittent claudication, where possible.
- The graded endurance exercise should be done three to five days a week.
- Prior to initiating walking or cycling, the patient should perform mild warm-up and stretching activities. Warm-up activities could include active ankle and toe pumping exercises
- Aerobic Exercise
Precautions and contraindications for participation in a walking program for patients with chronic arterial insufficiency are
Precautions
- Avoid exercising outside when the weather is very cold.
- Wear properly fitting shoes, have enough padding, and don't cause skin irritation.
- Follow each exercise session carefully to inspect the feet for evidence of skin irritation.
- If leg pain increases rather than decreases over time, discontinue a walking program.
Contraindications
- Skin irritation, ulceration, wound, or feet fungal infection
- Resting leg pain due to advanced vascular disease



Comments
Post a Comment